Leslie Capo
Office: 504-568-4806
Cell: 504-452-9166
lcapo@lsuhsc.edu
Related

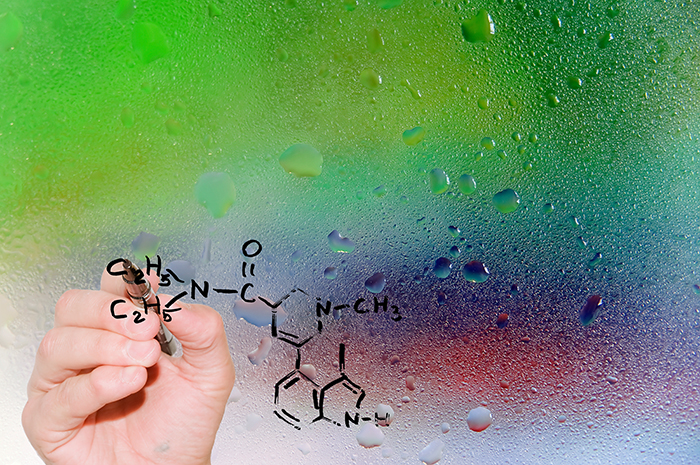
To conduct this research, the Nichols lab developed a powerful new method to sort brain cells using antibodies specific for cells in the nucleus, cytoplasm, or extracellular membranes. Before, cells from the brain could be sorted using antibodies that recognized proteins only in the cell’s nucleus, significantly restricting the variety of cell types that could be purified. Once the researchers had the different types of cells highly purified from one another, they were able to catalog the different genes they turned on. Being able to sort cells from one another by the proteins present in their cytoplasm or on their outer membranes, combined with gene profiling, allowed the researchers to perform a detailed analysis of brain tissue that was not previously possible.
In terms of translating these discoveries to therapies, it is a leap forward towards understanding cellular mechanisms in the living brain underlying not only the ability of psychedelics to potentially treat anxiety, depression, and addiction, but of normal cognitive processes as well.
The research team also included David A. Martin, who graduated from LSU Health New Orleans School of Graduates Studies with a PhD in Pharmacology and Experimental Therapeutics on May 19, 2016.
This work was partially funded by NIH grants R01MH083689, P30GM106392, and the Heffter Research Institute.
